Modified Bentall’s procedure for annuloaortic ectasia with severe left ventricular systolic dysfunction- A case study of the patient with Marfan syndrome
- Article
- Article Info
- Author Info
Introduction
The term annuloaortic ectasia refers to an aneurysm of the aortic root accompanied by dilation of the annulus of the aortic valve and aortic valve incompetence as the result of cystic medial degeneration (i.e., the tunica media of the aorta becomes less elastic as fibers break down). This may be a result of the aging process; hypertension; connective tissue disorders, such as Marfan’s syndrome; or other unknown factors [1,2]. The pathologic changes in the ascending aorta can cause aneurysmal dilation of the aortic root, which can affect the ability of the aortic valve cusps to close, leading to valve incompetence and aortic regurgitation. Annuloaortic ectasia frequently is an indication of surgical aortic root replacement.
A composite valve graft aortic root replacement (CGR), first reported by Bentall and DeBono in 1968, [3] has been applied to a variety of aortic root diseases. During the last two decades, CGR, with various technical modifications, [4-6] has become a standard procedure for aortic root disorders. Currently, a full-thickness “button” of the aorta surrounding the coronary ostia (i.e., where the proximal coronary arteries attach to the aorta) is removed, making it easier to implant the proximal coronary arteries into the aortic vascular graft, referred to as the “aortic button technique” [7]. The modified Bentall technique, which was reported by Svensson in 1992, is an aortic root composite valve graft replacement involving reimplantation of the left coronary ostium with a long-interposed graft wrapping behind the composite graft [8].
Case Presentation
A 40-year-old male, previously fit and well, presented with shortness of breath for the past three years. He also experienced palpitation and occasional mild central chest pain for the same duration. His physical examination was remarkable for Marfan’s Syndrome and aortic regurgitation. His blood test revealed raised NT pro-BNP more than a hundred times of normal level alongside severe aortic regurgitation with dilated aortic root (aortic annulus 33 mm,
aortic sinus 78 mm, Sinutubular junction 50 mm, arch of Aorta 24 mm) associated with severe left ventricular systolic dysfunction (LVEF-27%) on echocardiography [Figure 1].
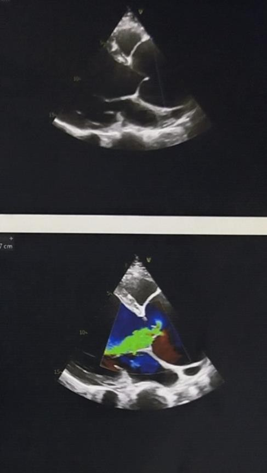
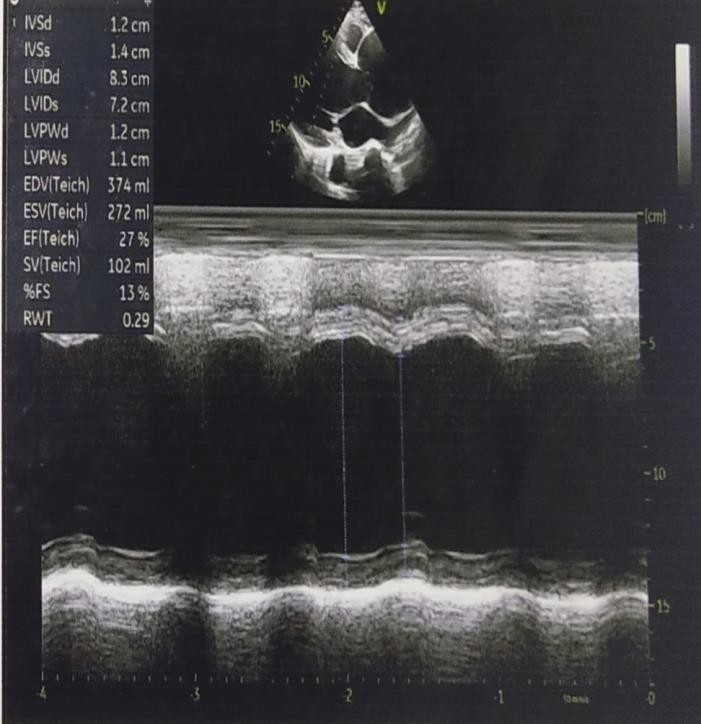
Figure 1: Preoperative echocardiography: (On Left) the PLAX view of transthoracic echocardiography demonstrates the dilatation of the aortic root and the green color flow (Jet flow) of severe aortic regurgitation to the left ventricle. (On Right) PLAX view showing severe left ventricular systolic dysfunction (LVEF-27%).
Further, his CT Aortogram showed aneurysmal dilatation of ascending aorta and aortic root (Root 56 mm, Sinutubular junction 87 mm, ascending Aorta 80 mm, arch of Aorta 29 mm, DTA 20 mm) [Figure 2].

Figure 2: Preoperative CT Aortogram: showing Annuloaortic ectasia (with measurement).
His CT coronary angiogram was reported as a non-calcified plaque with mild narrowing (40-50%) seen in proximal LAD, proximal RCA, and LCX. However, he is a non-smoker and a non-drinker. His family history is not significant for Marfan’s syndrome and heart disease [Figure 3].
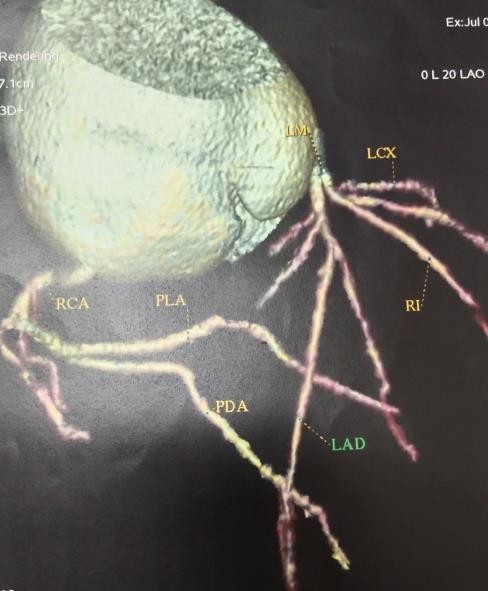
Figure 3: Preoperative CT coronary angiogram: showing non-significant ostial stenosis (40-50%) in major three coronary arteries.
After admission to the National Institute of Cardiovascular Disease (NICVD, Dhaka), he was optimized for one and a half months. Then, he was transferred to OR for surgical correction using a modified Bentall’s procedure. The Anaesthsist places pressure monitoring lines (i.e., radial arterial line, central line) for hemodynamic monitoring during the intraoperative and immediate postoperative periods. With all aseptic precautions, under general anaesthesia, the patient was positioned properly and was operated through median sternotomy.
After opening the pericardium, the aortic root and ascending aorta were found severely dilated. CPB was established through the aortic (Just proximal to the innominate artery) and a two-stage single venous cannula. However, when the desired ACT was achieved, an aortic cross-clamp was applied, and a cold Del Nido cardioplegia solution was infused into the aortic root. Cold saline slush is applied topically to the heart to assist in myocardial protection. Once asystole is obtained, the surgeon cut the aorta transversely, proximal to the innominate artery. The aneurysmal portion of the aorta was excised and the valve following the openings of the coronary ostia concerning their position to the annulus was inspected. The coronary ostia were detached from the aorta with rims of aortic tissue.
Subsequently, the aortic valve was replaced by a 24 mm ATS bi-leaflet mechanical valve followed by an aortic root, and ascending aorta was replaced with a 30 mm tube conduit, sutured with continuous polypropylene sutures. The coronary arteries were re-implanted through button incisions in the valve conduit. Then the tube graft was cut to the appropriate length and the distal portion of the tube graft was anastomosed to the distal aorta using a continuous polypropylene suture to complete the repair. After deaeration, the CPB was discontinued gradually and the patient was weaned to normal sinus rhythm with minimum inotrope. When the reversal of the anticoagulant effect of the heparin was confirmed, decannulation was done. Two temporary pacing wires -one on the right ventricle and one on the skin were placed. A straight, 32-Fr chest tube into the left pleura and a straight, 32-Fr chest tube into the patient’s mediastinum was introduced and connected to a closed, chest-drainage system for postoperative monitoring. However, the total CPB time for this patient was 349 min, and the total X clamp time was 285 min. After achieving haemostasis, the chest wound was closed [Figure 4].
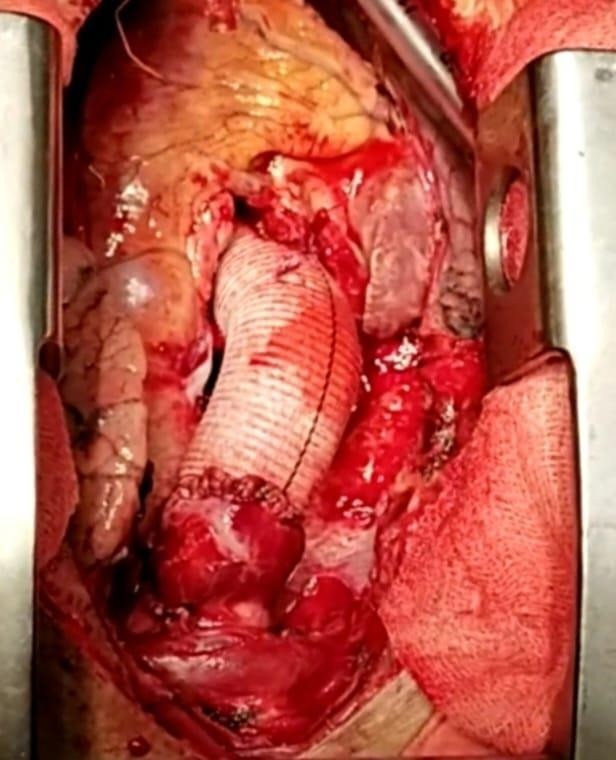
Figure 4: (Intraoperative) after composite mechanical valve and tube graft replacement.
He was transferred to ICU with minimum inotropes and was extubated 9 hours after shifting to the ICU having less than 100 ml blood loss in the chest drain tube. The patient’s postoperative period in the ICU was eventless. Post-operative echocardiography showed a well-seated and normally functioning prosthetic Aortic valve. On the 4th POD, an INR was 1.42 at 2.5 mg warfarin. Finally, the patient was discharged on the 7th POD at 5mg of warfarin.
Discussion
The aortic root dilates due to increased aortic stiffness and pulse wave velocity, enhanced by fibrillin fragmentation as a result of underlying FBN1 mutation [9] The current results suggested that Marfan syndrome was one of the significant predictors of late deaths. In the case of Marfan syndrome, surgery is indicated when the aortic root or ascending aortic diameter is >50 mm (Class I). The high incidence of aortic dissection and an aneurysm of the residual aorta, or subsequent operations can potentially increase the late mortality in Marfan patients. In fact, in the current series, the incidence of reoperation on the residual aorta was significantly higher in Marfan patients (27 patients; 29%) than in non-Marfan patients (5%). The incidence of graft detachment and coronary ostial true aneurysm were significantly high in Marfan patients. To reduce these complications, a direct button technique can be the most favorable technique, especially in Marfan patients [10].
The direct button technique is widely utilized and has reduced the rate of reoperation on the ascending aorta or aortic valve after a CGR (0% to 19% at 3 to 10 years).4,5,[11-13] The current data support the efficacy of the graft interposition technique with nearly the same long-term reliability as the direct button technique.5 In aortic root composite valve graft replacement, the procedures for reconstructing the coronary Ostia are very important for influencing the long-term outcome as well as the early operative results [11,14,15].
Although recent studies report an excellent early survival rate for a proximal reoperation after a CGR, ranging between 70% and 86%, [10,16,17] the Bentall procedure has potential complications which include graft infection, stoke caused by embolization of atherosclerotic plaques during surgery or coronary insufficiency secondary to a coronary artery implanted into the graft becoming kinked.7 During weaning from cardiopulmonary bypass or achieving hemostasis, kinking of the reconstructed coronary arteries or bleeding from the coronary ostial anastomosis can cause an intraoperative hemodynamic problem to be fatal. During long-term follow-up, complications associated with deterioration such as kinking of the graft with impaired coronary perfusion or coronary ostial pseudoaneurysm formation can develop [18,19] Therefore, surgeons should be ready to choose an appropriate coronary reconstruction technique to avoid fatal complications and improve the outcome [20].
Conclusion
The Modified Bentall’s procedure can be considered a safe, reliable, and justifiable method for various aortic root diseases even though the patient has ischemic heart diseases and severely decreased left ventricular systolic dysfunction. However, surgeons, especially in our country, can become more confident about using this technique, particularly for complicated patients such as our case.
Follow-up
At one month, the patient was alive, without evidence of infection, myocardial infarction, and thromboembolism, asymptomatic, and well.
References
- Seifert PC (2002) Cardiac Surgery: Perioperative Patient Care. Mosby.
- Beese-Bjurstrom S (2004) Hidden danger: Aortic aneurysms & dissections. Nursing 34: 36-42.
- Bentall H, De Bono A (1968) A technique for complete replacement of the ascending aorta. Thorax 23: 338-339.
- Kouchoukos NT, Wareing TH, Murphy SF, Perrillo JB (1991) Sixteen-year experience with aortic root replacement. Results of 172 operations. Annals of surgery 214: 308.
- Svensson LG, Crawford ES, Hess KR, Coselli JS, Safi HJ (1992) Composite valve graft replacement of the proximal aorta: comparison of techniques in 348 patients. The Annals of thoracic surgery 54 :427-439.
- Cabrol C, Pavie A, Gandjbakhch I, Villemot JP, Guiraudon G, et al. (1981) Complete replacement of the ascending aorta with reimplantation of the coronary arteries: new surgical approach. J Thorac Cardiovasc Surg 81: 309-315.
- Cherry C, DeBord S, Hickey C (2006) The modified Bentall procedure for aortic root replacement. AORN 84: 51-70.
- Nakahira A, Shibata T, Sasaki Y, Hirai H, Hattori K, et al. (2009) Outcome after the modified Bentall technique with a long-interposed graft to the left coronary artery. Ann thorac Surg 87: 109-115.
- Robinson PN, Arteaga-Solis E, Baldock C, Collod-Béroud G, Booms P, et al. (2006) The molecular genetics of Marfan syndrome and related disorders. J Med Genetics 43: 769-87.
- Kazui T, Yamashita K, Terada H, Washiyama N, Suzuki T, et al. (2003) Late reoperation for proximal aortic and arch complications after previous composite graft replacement in Marfan patients. Ann thorac Surg 76: 1203-1207.
- Hagl C, Strauch JT, Spielvogel D, Galla JD, Lansman SL, et al. Is the Bentall procedure for ascending aorta or aortic valve replacement the best approach for long-term event-free survival? Ann thorac Surg 76: 698-703.
- Alexiou C, Langley SM, Charlesworth P, Haw MP, Livesey SA, et al. Aortic root replacement in patients with Marfan’s syndrome: the Southampton experience. Ann thorac Surg 72: 1502-1507.
- Panos A, Amahzoune B, Robin J, Champsaur G, Ninet J (2001) Influence of technique of coronary artery implantation on long-term results in composite aortic root replacement. Ann thorac Surg 72:1497-501.
- Stalder M, Staffelbach S, Immer FF, Englberger L, Berdat PA, et al. (2007) Aortic root replacement does not affect outcome and quality of life. Ann thorac Surg 84: 775-781.
- Sioris T, David TE, Ivanov J, Armstrong S, Feindel CM (2004) Clinical outcomes after separate and composite replacement of the aortic valve and ascending aorta. J Thorac Cardiovasc Surg 128: 260-265.
- LeMaire SA, DiBardino DJ, üneyt Köksoy C, Coselli JS (2002) Proximal aortic reoperations in patients with composite valve grafts. Ann thorac Surg 74 :S1777-1780.
- Lepore V, Larsson S, Bugge M, Mantovani V, Karlsson T (1996) Replacement of the ascending aorta with composite valve grafts: long term results. J Heart Valve Dis 5: 240-246.
- Dossche KM, de la Rivière AB, Morshuis WJ, Schepens MA, Bal ET, et al. Treatment of impaired coronary blood flow after aortic root replacement with human tissue valves. J Thorac Cardiovasc Surg 117: 1034-1035.
- Erkut B, Ceviz M, Becit N, Gündogdu F, Unlü Y, et al. (2007) Pseudoaneurysm of the left coronary ostial anastomoses as a complication of the modified Bentall procedure diagnosed by echocardiography and multislice computed tomography. In The heart surgery forum 10: 191-192.
- Milano AD, Pratali S, Mecozzi G, Boraschi P, Braccini G, et al. (2003) Fate of coronary ostial anastomoses after the modified Bentall procedure. Ann thorac Surg 2003 75: 1797- 801.
*Corresponding author: Dr. Md. Salahuddin Rahaman, Department of Cardiac Surgery, National University Hospital (NUH), Singapore. E-mail: docmd.sal@gmail.com, Telephone: (+65)83751284.
Citation: Dr Salahuddin Rahaman (2023) Modified Bentall’s procedure for annuloaortic ectasia with severe left ventricular systolic dysfunction- A case study of the patient with Marfan syndrome. Int J Card Carth Sur 2: 01.
Received: Nov 28, 2023; Accepted: Dec 08, 2023, Published: Dec 14 2023
Copyright: © 2023 Dr. Salahuddin Rahaman. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits un-restricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Md. Salahuddin Rahaman1, Iram Shahazadi2, Md. Kamrul Hasan3, Sanjay Kumar Raha4
1Department of Cardiac Surgery, National University Hospital (NUH), Singapore
2Dhaka Medical College Hospital (DMCH), Dhaka, Bangladesh
3Department of Cardiac Surgery, National Institute of Cardiovascular Diseases (NICVD), Dhaka, Bangladesh
4Department of Cardiac Surgery, National Institute of Cardiovascular Diseases (NICVD), Dhaka, Bangladesh