Oligometastatic Renal Cell Cancer
- Article
- Article Info
- Author Info
Introduction
Kidney cancer, particularly renal cell carcinoma (RCC), ranks among the top 10 most prevalent cancers in the United States, projected to affect around 81,800 individuals and contribute to 14,890 deaths in the year 2023. RCC constitutes most kidney cancer cases, where 15% of patients manifest metastases upon presentation, and an additional 20% develop metastatic disease post-treatment for localized conditions[1].
Metastatic RCC (mRCC) spans a wide spectrum of aggressiveness, as evidenced by the International Metastatic Database Consortium’s risk stratification. Patients classified as poor-risk have a survival rate of under one year, while those with favorable-risk may experience a gradual progression over several years. Oligometastatic RCC (OM-RCC) describes cases with a limited number of detectable metastatic lesions at initial presentation, typically numbering five or fewer. However, the incidence of OM-RCC remains inadequately studied.
While some patients may be genuinely oligometastatic with detectable lesions as their only metastases, it is presumed that many harbor undetectable micro metastatic disease. Consequently, depending on the rate of metastatic site progression, local therapy alone or in combination with systemic therapy may offer benefits. Although IMDC risk stratification is not specifically tailored to OM-RCC, it can be applied by categorizing patients based on the risk of distant micro metastasis and disease progression rate. This classification aids in determining future progression probability at distant sites, thus informing decisions on local versus combined treatment approaches. Patients with a slower progression may even be candidates for surveillance[2, 3].
OM-RCC stands apart from oligoprogressive disease, where RCC patients experience progression only in limited sites while receiving ongoing systemic therapy. Despite differences, both oligometastatic and oligoprogressive diseases share overlapping management principles that encompass a multimodality approach[4].
Significant progress has been made in the surgical, radiation, and medical management of RCC over the past decade. This review offers an overview of contemporary multidisciplinary management strategies for OM-RCC. In recent times, therapeutic advancements in head and neck cancer have contributed to lower death risks from recurrences and metastatic spread. While new systemic modalities harness immune cells to combat cancer, increasing attention is directed towards local ablative methods that show promise against distant lesions. Specifically, cases with slowly growing metastases seem particularly suited for these therapies.
Objectives and Scope of the Review
This review aims to comprehensively explore the nature of oligometastatic renal cancer from an updated perspective. Throughout the article, we will examine key aspects related to its correct diagnosis, therapeutic options, and associated prognosis. Through the assessment of recent clinical studies, we will review emerging strategies that are transforming the way we approach this challenging subset of renal cancer.
To achieve a thorough understanding, we will delve into molecular aspects, advanced imaging approaches, and targeted therapies that are at the forefront of oligometastatic renal cancer treatment. Additionally, we will consider the importance of patient selection, multidisciplinary coordination, and evidence-based decision-making in the care process.
Throughout this review, emphasis will be placed on the significance of collaboration among oncologists, surgeons, radiation therapists, and other healthcare professionals to provide comprehensive and personalized care to patients with oligometastatic renal cancer. With updated information and solid evidence, this review looks to offer a useful guide for medical professionals involved in the care of these patients, thereby promoting improvements in long-term quality of life and prognosis.
Fundamentals of Renal Cancer and Metastasis
Renal cancer, known as renal cell carcinoma (RCC), is a type of neoplasm originating from kidney cells and accounts for 2-3% of all cancers globally. Despite advances in diagnosis and treatment, RCC is still a challenging disease due to its potential to develop metastasis, even in initial stages.
Characteristics of Renal Cancer and its Propensity for Metastasis
RCC is characterized by its histological and molecular heterogeneity, complicating its diagnosis and treatment. The most common histological type is clear cell carcinoma, followed by papillary carcinoma and chromophobe carcinoma. A notable feature of RCC is its potential to invade the renal vein and the vena cava, increasing the risk of tumor dissemination even before clinical manifestation of metastatic disease[5].
Process of Metastasis in Renal Cancer
Metastasis is a complex process in which tumor cells spread from the primary site to distant organs and tissues. In the case of RCC, metastases often affect the lungs, bones, liver, and central nervous system. Cell invasion and migration are helped by genetic and epigenetic alterations that promote the acquisition of more aggressive phenotypes[5].
Clinical Importance of Oligometastatic Disease
Oligometastatic disease in RCC is a clinically significant entity. Unlike extensive metastatic disease where multiple organs are involved, oligometastatic disease is characterized by a limited number of metastases, usually one to three sites. This presentation offers opportunities for more aggressive and focused therapeutic approaches [Figure1].
Figure 1: Oligometastatic kidney cancer
Accurate identification of oligometastatic disease has important implications in treatment planning. Strategies such as surgery and targeted radiation therapy may be considered for selected patients, aiming to remove or control metastatic lesions[6, 7]. Additionally, oligometastatic disease can serve as a platform for evaluating novel systemic therapies, including immunotherapies and targeted therapies, which may redefine the treatment landscape in the future.
In summary, RCC presents a unique propensity for metastasis that can impact the clinical course of patients. Oligometastatic disease emerges as a clinically relevant entity, offering opportunities for more focused and optimized therapeutic interventions. Understanding the fundamentals of renal cancer and its relationship with metastasis is essential to effectively address this disease and improve clinical outcomes.
Accurate Diagnosis and Evaluation
Utilization of Advanced Medical Imaging for Diagnosis
The precise diagnosis of oligometastatic renal cancer requires the use of advanced imaging techniques that enable early detection and accurate assessment of metastatic lesions. Medical imaging plays a pivotal role in identifying metastatic sites as well as determining their size, shape, and location. Among the techniques employed, computed tomography (CT) and magnetic resonance imaging (MRI) are key tolos [8, 9].
CT is widely utilized to evaluate the abdomen and chest for metastases in organs such as the lungs, liver, and lymph nodes [8, 9]. MRI, on the other hand, can provide detailed information about the extent of lesions, especially in the central nervous system and anatomically complex areas. The combination of these techniques can enable a more comprehensive and precise assessment of metastatic lesions in oligometastatic renal cancer [9].
Assessment of Extent and Location of Metastases
Once metastatic lesions are identified, it is essential to assess their extent and location to plan treatment appropriately. In addition to CT and MRI, other techniques such as positron emission tomography (PET-CT) can provide functional information about the metabolic activity of lesions. This can be particularly useful in differentiating between active tumor tissue and benign changes[10-12].
Assessing the extent of metastases also involves considering the relationship of the lesions with critical structures, such as blood vessels or the nervous system. This information is crucial in determining the feasibility of surgical resection or the application of focused radiation therapy. Decision-making based on the precise location of lesions can minimize side effects and enhance clinical outcomes[11-13].
Differentiation Between Oligometastatic and Advanced Metastatic Disease
Distinguishing between oligometastatic and advanced metastatic disease is pivotal in determining the most appropriate treatment options. Oligometastatic disease, characterized by a limited number of metastatic sites, often presents a more favorable prognosis, and can be addressed with more aggressive approaches, such as surgery or focused radiation therapy. On the other hand, in advanced metastatic disease where multiple organs are affected, systemic and palliative therapies may be considered to control symptoms and enhance quality of life.
In summary, accurate diagnosis and comprehensive evaluation of metastatic lesions are foundational pillars in the care of oligometastatic renal cancer. Advanced medical imaging plays an essential role in early detection, assessing the extent, and differentiating between oligometastatic and advanced metastatic disease, allowing for more precise and effective therapeutic planning [12].
Therapeutic Strategies in Oligometastatic Renal Cancer
Cytoreductive Nephrectomy in the Era of Metastatic Renal Cell Carcinoma: A Comprehensive Exploration
The significance of Cytoreductive Nephrectomy (CN) in the management of metastatic renal cell carcinoma (mRCC) cannot be overstated. In this comprehensive review, we embark on a journey through the diverse dimensions of CN, dissecting its rationale, contemporary indications, and its pivotal role in delaying systemic therapy, enhancing its impact through adjunctive use, and providing symptom palliation [7].
Modern therapeutic paradigms have reshaped the indications for CN. We uncover the intricate scenarios where CN emerges as a pivotal consideration, including instances where metastatic disease is amenable to active surveillance (AS), limited metastatic disease that aligns with metastasis-directed therapy (MDT), IMDC risk factor profiles, oligoprogressive disease post-systemic therapy, and scenarios of pronounced local symptoms that necessitate palliation [2].
Beyond its surgical implications, CN’s potential to postpone systemic therapy offers intriguing possibilities. We unravel this aspect, shedding light on CN’s ability to buy time through AS, thereby minimizing systemic therapy-related toxicity. This calculated approach presents a nuanced understanding of CN’s influence on disease progression and patient well-being.
CN’s role as an accompaniment to systemic therapy has evolved significantly. Pioneered during the cytokine era and carried into the targeted therapy epoch, CN’s contribution to patient outcomes has evolved. By delving into seminal trials like CARMENA and SURTIME, we glean insights into CN’s potential benefits, while recognizing the impact of individual patient characteristics [14-17].
Beyond its role as a therapeutic tool, CN finds its place in symptom palliation for mRCC patients. We explore how CN can alleviate the burden of local symptoms, restoring patient comfort and quality of life. Furthermore, we delve into alternative interventions, such as angioembolization, stereotactic body radiotherapy (SBRT), and systemic therapy, for tailored symptom management [18].
As metastasis-directed therapy (MDT) gains prominence, we unravel its intricacies and dynamic potential. With a spotlight on ablative techniques like SBRT and the confluence of systemic therapy, MDT emerges as an ally in controlling metastatic lesions. We dissect its evolving role in disease control, quality of life enhancement, and its synchronization with systemic interventions [18, 19].
In summation, CN stands as a cornerstone in managing metastatic renal cell carcinoma. This review encapsulates its dynamic role in delaying systemic therapy, synergizing with systemic treatments, and offering symptom relief. The burgeoning field of metastasis-directed therapy adds a fresh perspective to mRCC management. By presenting contemporary insights and ongoing research, this review fosters informed decision-making and optimal care for patients navigating the complexities of metastatic renal cell carcinoma.
Surgery as an Option for Metastatic Lesion Resection
Surgery has emerged as a significant therapeutic strategy in the treatment of oligometastatic renal cancer, especially when metastatic lesions are potentially resectable[14]. Surgical resection of metastases can offer substantial benefits by eliminating sources of disease and alleviating local symptoms. Appropriate patient selection for surgery is crucial and should be based on a comprehensive assessment of the extent and location of lesions, as well as the overall health of the patient[16].
In certain cases, patients who present with only a solitary or a small number of distant metastases can experience extended survival through nephrectomy combined with the surgical excision of these metastatic sites [16]. Recent research suggests that even individuals with brain metastases have shown comparable outcomes through this approach. This strategy tends to be most effective when patients exhibit a substantial disease-free interval between their initial nephrectomy and the emergence of metastatic lesions[7, 14].
Targeted Radiation Therapy for Metastases
Radiation therapy has evolved as an effective therapeutic strategy for oligometastatic renal cancer. Targeted radiation therapy, also known as stereotactic body radiation therapy (SBRT), allows the precise delivery of high doses of radiation to metastatic lesions while minimizing damage to surrounding tissues. This technique is particularly useful in cases where surgery is not a viable option due to lesion location or the patient’s clinical condition[18].
Stereotactic Body Radiotherapy (SBRT): A Comprehensive Exploration of a Revolutionary Non-Invasive Precision Radiation Technique
Stereotactic Body Radiotherapy (SBRT) has emerged as a transformative technique in the realm of radiation oncology[18, 19]. This review delves into the multifaceted dimensions of SBRT, tracing its evolution from its roots in stereotactic radiosurgery for brain tumors. We explore the distinctive attributes of SBRT that have led to its prominence as a non-invasive, highly conformal treatment modality, with particular emphasis on its application in the context of renal cell carcinoma (RCC) and metastatic lesions.
SBRT Unveiled: A Precision Approach
SBRT stands as an exceptional non-invasive therapy, offering the delivery of high doses per fraction with remarkable precision. Its unique ability to target metastatic lesions with image-guided accuracy while safeguarding surrounding normal tissues has ushered in a new era in radiation therapy. Notably, SBRT’s potency is augmented by its concise treatment schedule, typically requiring only five or fewer fractions[6, 19].
Redefining RCC Radioresistance: Overcoming Challenges
Renal cell carcinoma (RCC) is often characterized by radioresistance, especially when treated with conventional fractionation. SBRT has emerged as a promising solution to this challenge, with its potential to deliver potent doses and achieve effective local control, thereby offering a means to overcome the radioresistance often encountered in RCC [6].
The Spectrum of Application
Brain metastases are a common manifestation in RCC, leading to significant morbidity and mortality. SBRT has emerged as a crucial tool in addressing these metastatic lesions, offering a non-invasive, precise alternative to surgical resection and conventional radiotherapy. Studies have shown that untreated brain metastases are associated with poor survival, while SBRT offers the potential for extended survival and improved outcomes[20, 21].
Optimizing Treatment Strategies
Multiple studies have explored the efficacy of SBRT in patients with RCC brain metastases. The combination of whole-brain radiotherapy (WBRT) and SBRT has demonstrated the potential to enhance survival rates in this patient cohort. Furthermore, studies have highlighted the success of SBRT in patients with solitary lesions and have underscored its role in achieving local control and extending survival[22, 23].
Exploring Technical Considerations
The anatomical proximity of the adrenal gland and kidney necessitates a nuanced approach to delivering SBRT to these sites. SBRT emerges as a feasible option for primary RCC and adrenal metastases, especially when surgical intervention is suboptimal. Studies have demonstrated SBRT’s potential to provide excellent local control, while its standardized dosimetric planning and quality assurance protocols ensure reproducibility and safety.
Safety and Outcomes
Studies evaluating SBRT’s impact on renal function have shown encouraging results, with low rates of dialysis and minimal renal dysfunction. Emerging data suggests that even patients with pre-existing renal impairment can benefit from SBRT without detrimental effects on renal function. Studies have also highlighted the favorable toxicity profile of SBRT, with minimal severe toxicities reported.
Future Directions
As the field of SBRT continues to evolve, the role of this non-invasive technique in the management of RCC and metastatic lesions remains a topic of active investigation. Ongoing studies aim to further refine treatment protocols, establish safe organ-at-risk constraints, and explore the potential of SBRT to replace surgical interventions in select patient populations [23].
In conclusion, SBRT has ushered in a new era of precision radiation therapy, redefining the treatment landscape for RCC and metastatic lesions. Its ability to deliver high doses with precision, achieve effective local control, and minimize toxicities makes it an invaluable tool in oncology. As research and clinical experience expand, SBRT’s impact on patient outcomes is set to grow, offering a promising future for patients navigating the complexities of RCC and metastatic disease [Figure 2] .
Figure 2: Oligometastatic kidney cancer can be treated with stereotactic body radiation (SBRT).
Targeted Systemic Therapies and their Impact on Disease Control
The development of targeted systemic therapies has revolutionized the treatment of oligometastatic renal cancer. Tyrosine kinase inhibitors (TKIs) and immune checkpoint inhibitors are prominent examples of therapies that have demonstrated efficacy in this patient population[24]. TKIs such as sunitinib and pazopanib have shown their ability to control tumor growth and improve survival. Immunotherapy therapies like nivolumab and ipilimumab have demonstrated their capacity to stimulate the patient’s immune response and enhance disease control.
The choice of systemic therapy should be based on individual considerations, such as the tumor’s genetic profile, the patient’s overall health, and their preferences. The combination of systemic therapies with local approaches, such as surgery or radiation therapy, can further enhance disease control in oligometastatic renal cancer [25].
In summary, therapeutic strategies in oligometastatic renal cancer have evolved significantly. Surgery, targeted radiation therapy, and targeted systemic therapies play a pivotal role in disease control and improvement of patients’ quality of life [25]. Optimal therapeutic strategy selection should be individualized and based on a multidisciplinary assessment of each case.
Multidisciplinary and Personalized Approach
Importance of Collaboration Among Oncologists, Surgeons, and Radiation Therapists
The management of oligometastatic renal cancer requires close and coordinated collaboration among different medical specialties. Teamwork among medical oncologists, surgeons, and radiation therapists is essential to ensure that patients receive the most appropriate therapeutic approach. The complementary expertise and knowledge of these specialties allow for a comprehensive analysis of each case, considering available therapeutic options and the patient’s clinical characteristics.
Evidence-Based and Clinical Situation-Driven Decision Making
The approach to oligometastatic renal cancer benefits from evidence-based decision making tailored to each patient’s clinical situation. Current clinical guidelines and research provide the foundation for selecting the most effective therapeutic strategies. However, it is essential to consider individual factors such as the patient’s overall health, the location and extent of metastatic lesions, as well as personal preferences.
Personalized Approach for Each Patient
The heterogeneous nature of oligometastatic renal cancer demands a personalized approach to each patient’s treatment. Everyone may have diverse needs and clinical considerations, requiring a comprehensive and thoughtful evaluation. Selecting the appropriate therapeutic strategy should consider not only the expected clinical response but also the patient’s quality of life and preferences.
The personalized approach also extends to the identification of specific biomarkers and genetic mutations that may influence the response to targeted therapies. Precision medicine allows tailoring treatment to the genomic characteristics of the tumor, thereby enhancing effectiveness and reducing side effects.
In summary, a multidisciplinary and personalized approach is crucial in the treatment of oligometastatic renal cancer. Collaboration among different medical specialties, evidence-based and clinical situation-driven decision making, and a personalized approach for each patient are fundamental pillars to achieve the best therapeutic outcomes and improve patients’ quality of life.
Prognosis and Quality of Life
Comparison of Prognosis in Oligometastatic and Advanced Metastatic Disease
The prognosis in oligometastatic renal cancer significantly differs from advanced metastatic disease. The presence of a limited number of metastases in oligometastatic disease suggests a less aggressive biological behavior and a more favorable prognosis compared to advanced metastatic disease, which involves multiple metastatic sites. Patients with oligometastatic disease may benefit from more aggressive and targeted therapeutic strategies such as surgery and radiation therapy, contributing to increased survival and disease control.
Impact on Patients’ and Families’ Quality of Life
The diagnosis of oligometastatic renal cancer has a significant impact on both patients’ and their families’ quality of life. Uncertainty about the disease course and treatment decisions can lead to anxiety and emotional stress. Moreover, physical symptoms and treatment side effects can affect functional capacity and overall well-being.
Management of Side Effects and Emotional Well-being
The management of side effects and emotional well-being are essential components of comprehensive management of oligometastatic renal cancer. Treatments such as surgery, radiation therapy, and systemic therapies can be associated with side effects that impact quality of life. Addressing symptoms and implementing strategies to minimize side effects are crucial to ensure patient comfort and satisfaction.
Patients’ and families’ emotional well-being should be addressed through a multidisciplinary approach. Psychological support and open communication with the medical team are crucial to help patients cope with anxiety, fear, and other emotional challenges associated with the diagnosis and treatment of oligometastatic renal cancer.
In summary, prognosis, and quality of life in oligometastatic renal cancer are critical factors in comprehensive patient care. Comparing the prognosis between oligometastatic and advanced metastatic disease, understanding the impact on patients’ and families’ quality of life, and managing side effects and emotional well-being should all be considered in therapeutic decision-making and long-term care planning.
Future Perspectives in Oligometastatic Renal Cancer
Advances in the Identification of Specific Therapeutic Targets
Continual advancements in understanding the biology of renal cancer are leading to the identification of specific therapeutic targets that could revolutionize the treatment of oligometastatic renal cancer. Current research is focused on identifying genetic and molecular alterations that drive the growth and spread of metastatic lesions. The development of therapies targeting these specific targets can enhance treatment effectiveness and minimize associated side effects.
Development of Immunotherapies and Combination Approaches
Immunotherapies, such as checkpoint inhibitors and modified T-cell therapies, are transforming the treatment landscape for a different type of cancers, including oligometastatic renal cancer. The ability to reinvigorate the patient’s immune response against tumor cells can be particularly valuable in this context. Clinical trials are underway to evaluate the efficacy and safety of these therapies in treating metastatic lesions.
Furthermore, the integration of therapeutic approaches is gaining attention within the medical community. The combination of systemic therapies with local approaches like surgery and radiation therapy can enhance therapeutic response and extend survival. Research in this area aims to determine the most effective combinations and optimal treatment sequencing to maximize clinical outcomes.
Role of Precision Medicine in Treatment Optimization
Precision medicine, based on the identification of specific biomarkers and genetic mutations, is emerging as a fundamental approach in optimizing treatments for oligometastatic renal cancer. The ability to identify unique molecular characteristics of the tumor allows for the selection of targeted therapies that are more effective for each patient. This can result in more effective treatment and a reduction in side effects associated with non-specific therapies.
In summary, the future perspectives in oligometastatic renal cancer are promising and driven by advances in the identification of specific therapeutic targets, the development of immunotherapies, and combination therapeutic approaches. Precision medicine will also play a key role in treatment optimization, enabling more personalized and effective care for patients.
Discussion
Clinical Studies and Significant Findings
Research in the field of oligometastatic renal cancer has yielded promising results over the years. Clinical studies have demonstrated that aggressive therapeutic strategies, such as surgery and focused radiation therapy, can enhance survival and disease control compared to more conservative approaches. Additionally, targeted therapies and immunotherapies are emerging as promising options for treating metastatic lesions.
The combination of systemic therapies and local approaches has also shown positive outcomes in terms of disease control and survival. Studies evaluating the optimal treatment sequence are shedding light on how to maximize therapeutic efficacy in oligometastatic renal cancer.
Current Challenges in the Treatment and Management of Oligometastatic Renal Cancer
Despite advancements, persistent challenges exist in the treatment and management of oligometastatic renal cancer. Early identification of metastatic lesions can be challenging due to the lack of clear symptoms. Furthermore, tumor heterogeneity can influence response to therapies, complicating the selection of effective treatments.
Managing the side effects of therapies and attending to patients’ quality of life remains areas of focus. While advanced therapies offer promising treatment options, they can also be associated with side effects that impact patients’ quality of life and emotional well-being.
Ethical Considerations and Patient-Centric Aspects
The approach to oligometastatic renal cancer also raises ethical considerations and patient-centric aspects. Decision-making should involve the patient and consider their values and preferences. Additionally, clear, and understandable communication about treatments, risks, and benefits is essential for patients to make informed decisions.
Comprehensive care should also address the psychological and emotional aspects of the disease. Psychological support and emotional care are crucial to help patients cope with anxiety, fear, and concerns associated with the diagnosis and treatment of oligometastatic renal cancer.
Conclusion
Oligometastatic renal cancer represents an ever-evolving field with significant clinical and future implications. Multidisciplinary and personalized care should be the central focus in clinical practice, enabling continuous improvement in therapeutic outcomes and patients’ quality of life. This review has underscored the importance of a collaborative approach among medical specialists, such as oncologists, surgeons, and radiation therapists, to address this unique presentation of renal cancer comprehensively and precisely.
Advances in identifying specific therapeutic targets have opened new doors for treating oligometastatic renal cancer. Precision medicine, based on a detailed understanding of each patient’s molecular characteristics, has allowed for the selection of more effective and personalized therapies. Furthermore, the development of immunotherapies, like checkpoint inhibitors, has revolutionized cancer therapy by enhancing the body’s immune response against cancer cells.
Precision medicine and advances in targeted therapies are transforming how we approach oligometastatic renal cancer. However, a comprehensive approach that considers multidisciplinary coordination and evidence-based decision making is required. Patients’ quality of life and emotional well-being must also be prioritized in the care process.
Continued progress in research and collaboration among different medical specialties are essential to enhance clinical outcomes and the quality of life for patients with oligometastatic renal cancer. The development of more effective and personalized therapies, as well as the identification of new therapeutic strategies, will continue to drive treatment optimization and long-term prognosis.
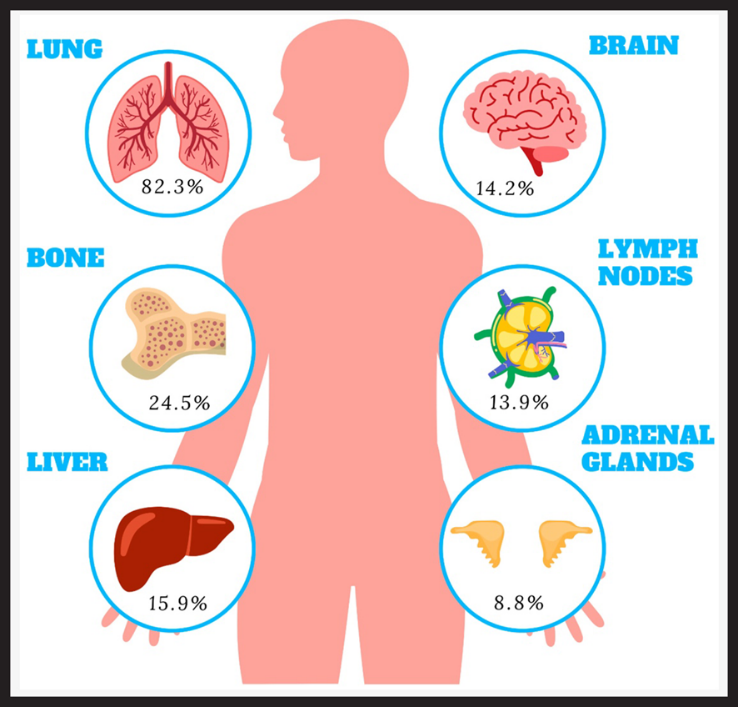
In summary, the constant evolution in understanding oligometastatic renal cancer and the application of multidisciplinary and personalized approaches are shaping a promising landscape in the fight against this disease. Ongoing research and collaboration among researchers and medical professionals are fundamental to advancing toward continuous improvement in clinical outcomes and the quality of life of patients with this unique presentation of renal cancer [Figure 3].
Figure 3: Main Messages and their Implication in Clinical Practice
| Main Message | Implications in Medical Practice |
| Oligometastatic renal cancer has limited metastases in number and location. | Identify oligometastatic cases for more aggressive and focused therapeutic approaches. |
| Collaboration among oncologists, surgeons, and radiation therapists is crucial. | Adopt a multidisciplinary approach in care to enhance therapeutic outcomes. |
| Early and accurate identification of metastatic lesions is crucial. | Use advanced medical imaging such as CT scans and MRI for early detection. |
| Precise diagnosis allows for appropriate treatment planning. | Evaluate the extent and location of metastases to determine treatment options. |
| Oligometastatic disease offers opportunities for aggressive, focused treatments like surgery and radiation. | Consider localized strategies for oligometastatic disease to improve survival. |
| Targeted systemic therapies like tyrosine kinase inhibitors and immunotherapies are effective in oligometastatic renal cancer. | Select therapies based on tumor genetic profile and patient’s overall health. |
| Precision medicine enables personalized treatments based on biomarkers and genetic mutations. | Use genomic information to optimize efficacy and reduce side effects of therapies. |
| Emotional well-being and quality of life must be considered in treatment. | Provide psychological support and emotional care to enhance patient and family well-being. |
| Advances in target identification and immunotherapies are transforming oligometastatic renal cancer treatment. | Stay informed about research and consider new treatment options. |
| Multidisciplinary collaboration and evidence-based decision-making are essential. | Embrace a comprehensive and coordinated approach to care for better clinical outcomes. |
| Continuous research and collaboration are crucial for improved clinical outcomes and quality of life. | Engage in research and collaborate with other professionals to advance oligometastatic renal cancer treatment. |
References
- Siegel RL, Miller D, Fuchs E, Jemal E et al, (2022) Cancer statistics. CA Cancer J Clin 2022. 72: 7-33.
- Heng, DY, Xie Wan, Regan M,Wood L, Agarwal N, et al, (2013) External validation and comparison with other models of the International Metastatic Renal-Cell Carcinoma Database Consortium prognostic model: a population-based study. Lancet Oncol 14: 141-148.
- Sun M, Cheng C, Masaru M, Richard Z, Piere I et al, (2011) Prognostic factors and predictive models in renal cell carcinoma: a contemporary review. Eur Urol 60: 644-661.
- Dason S, Lacuna K, Hannan k et al, (2023) State of the Art: Multidisciplinary Management of Oligometastatic Renal Cell Carcinoma. Am Soc Clin Oncol Educ Book 43: e390038.
- Capitanio U, Francesco M, (2016) Renal cancer. Lancet 387: 94-906.
- Ali M, Mooi J, Rana R, Hannan R, Siva S et al, (2022) The Role of Stereotactic Ablative Body Radiotherapy in Renal Cell Carcinoma. Eur Urol 82: 613-622.
- Bex A, Albiges L, Boorje L, Bensalah K, Lam B et al, (2018) Updated European Association of Urology Guidelines for Cytoreductive Nephrectomy in Patients with Synchronous Metastatic Clear-cell Renal Cell Carcinoma. Eur Urol 74: 805-809.
- Gires B, Khene E, Pierre B, Alimi Q, Benoit P, et al, (2019) Impact of routine imaging in the diagnosis of recurrence for patients with localized and locally advanced renal tumor treated with nephrectomy. World J Urol 37: 2727-2736.
- Bigot P, Khene z (2002) French AFU Cancer Committee Guidelines – Update 2022-2024: management of kidney cancer. Prog Urol 32:1195-1274.
- Airo Farulla et al, (2023) [(18)F]FDG PET/CT: Lung Nodule Evaluation in Patients Affected by Renal Cell Carcinoma. Tomography 9: 387-397.
- Rowe SP, Gorin MA, Hans J, Pomper G, Javadi S, et al, (2016) Detection of 18F-FDG PET/CT Occult Lesions With 18F-DCFPyL PET/CT in a Patient With Metastatic Renal Cell Carcinoma. Clin Nucl Med 41: 83-85.
- deSouza NM, Yan L, Chiti A, Lecouver F, Ken H, et al, (2018) Strategies and technical challenges for imaging oligometastatic disease: Recommendations from the European Organisation for Research and Treatment of Cancer imaging group. Eur J Cancer 91: 153-163.
- Rowe SP, Gorin MA, Szabo Z, E Allaf, Y Cho et al, (2015) Imaging of metastatic clear cell renal cell carcinoma with PSMA-targeted (1)(8)F-DCFPyL PET/CT. Ann Nucl Med. 29: 877-82.
- Bhanvadia, S, Pal SK (2018) Cytoreductive nephrectomy: questions remain after CARMENA. Nat Rev Urol 15: 530-532.
- Roussel E. Beuselinck, Albersen M (2021) Three Years After CARMENA: What Have We Learned? Eur Urol 80: 425-427.
- De Bruijn RE, Mulders P, Jewett A, Wagstaff J, Collette L et al, (2019) Surgical Safety of Cytoreductive Nephrectomy Following Sunitinib: Results from the Multicentre, Randomised Controlled Trial of Immediate Versus Deferred Nephrectomy (SURTIME). Eur Urol 76: 437-440.
- Zequi SC, Mulders P, Jewett P, (2020) Editorial Comment: Comparison of Immediate vs Deferred Cytoreductive Nephrectomy in Patients With Synchronous Metastatic Renal Cell Carcinoma Receiving Sunitinib: The SURTIME Randomized Clinical Trial. Int Braz J Urol, 46: 476.
- Siva S, Ali M, Correa (2022) JM 5-year outcomes after stereotactic ablative body radiotherapy for primary renal cell carcinoma: an individual patient data meta-analysis from IROCK (the International Radiosurgery Consortium of the Kidney). Lancet Oncol 23: 1508-1516.
- Onal C, Gular C, Hurmuz P, Oymak E, Yavas Cet al, (2022) Bone-only oligometastatic renal cell carcinoma patients treated with stereotactic body radiotherapy: a multi-institutional study. Strahlenther Onkol 198:940-948.
- Marandino L (2023) The role of stereotactic ablative body radiotherapy in renal cell carcinoma: focus on oligometastatic and oligoprogressive disease. Minerva Urol Nephrol 75: 260-264.
- Buti S, Bersanelli M, Leonetti L, Bruni A, Andreani S et al, (2020) Treatment Outcome of metastatic lesions from renal cell carcinoma underGoing Extra-cranial stereotactic body radioTHERapy: The together retrospective study. Cancer Treat Res Commun, 22: 100161.
- Magee DE, Wong JK, Correa AF (2022) Stereotactic Ablative Body Radiotherapy: ¿An Emerging Weapon in the Treatment Armamentarium for Renal Cell Carcinoma or a Potential Avenue for Overtreatment? Eur Urol 82: 623-624.
- Zhang Y, Zhang Y, Christie A, Courtney K, Bowman I et al, (2019) Stereotactic Ablative Radiation Therapy (SAbR) Used to Defer Systemic Therapy in Oligometastatic Renal Cell Cancer. Int J Radiat Oncol Biol Phys 105: 367-375.
- Lu X (2016) Oligometastatic state predicts a favorable outcome for renal cell carcinoma patients with bone metastasis under the treatment of sunitinib. Oncotarget 7: 26879-87.
- Liatsou E, Diamantis T, Malandrakis P, Maria G, Ioannis N, et al, (2023) Current status and novel insights into the role of metastasectomy in the era of immunotherapy. Expert Rev Anticancer Ther 23: 57-66.
*Corresponding author: Dr. María Natalia Gandur Quiroga, MD, M.sc Medical Oncology, Genitourinary Tumor Service, Instituto de Oncología “Ángel H. Roffo”. Universidad de Buenos Aires, Av. San Martín 5481. Buenos Aires Argentina, Tel: +54 (011) 5287-5356; Email: nataliagandur@gmail.com
Citation: Dr María Natalia Gandur Quiroga (2023) Oligometastatic Renal Cell Cancer. Arc Can Res Med 4: 013. DOI: https://doi.org/10.58735/acrmsi113
Received: Aug 21, 2023; Accepted: Oct 05, 2023, Published: Oct 08 2023
Copyright: © 2023 Dr María Natalia Gandur Quiroga. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits un-restricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
María Natalia Gandur Quiroga 1*, Ricardo Miguel Nardone ²*, Chi Liang Tsou²*
1*Medical Oncology, Genitourinary Tumor Service, Instituto de Oncología “Ángel H. Roffo”. Universidad de Buenos Aires, Av. San Martín 5481. Buenos Aires Argentina
2*Urologist, M.D. Department of Urology. Instituto de Oncología “Ángel H. Roffo”. Universidad de Buenos Aires, Av. San Martín 5481. Buenos Aires Argentina
*Corresponding author: Dr. María Natalia Gandur Quiroga, MD, M.sc Medical Oncology, Genitourinary Tumor Service, Instituto de Oncología “Ángel H. Roffo”. Universidad de Buenos Aires, Av. San Martín 5481. Buenos Aires Argentina, Tel: +54 (011) 5287-5356; Email: nataliagandur@gmail.com