Renal Metastasis in Carcinoma Pyriform Fossa treated with SBRT: A Case Report and a Brief Review
- Article
- Article Info
- Author Info
Abstract
Head and neck cancers are the most common cancers in male in India. The most common site of metastasis being lung. Isolated metastasis to the kidney is a rare phenomenon in head and neck cancers. This article highlights a 65 year old male with carcinoma pyriform fossa with lung and renal metastasis progressed on Palliative chemotherapy and immunotherapy was treated with Stereotactic Body Radiotherapy (SBRT) to left kidney.
Keywords
Pyriform fossa, SBRT, Carcinoma, Kidney, Palliative radiotherapy
Introduction
Laryngeal cancer is the seventh most common cause of cancer in males [1].The main modalities of treatment are surgery followed by chemo-radiotherapy or concurrent chemo-radiotherapy (CTRT). With advances in treatment, there is considerable improvement in the survival of the patients. Whenever the disease progresses, the patient receives some form of palliative treatment. The commonest site of metastasis from head and neck malignancies is to the lungs, liver, bones, adrenal glands and kidney. However, metastasis to the kidney is rare. This is the first reported case of carcinoma pyriform fossa (CA-PFS) post CTRT, progressing to involve the lung and kidney, treated with palliative stereotactic body radiotherapy (SBRT) to the kidney.
Case Report
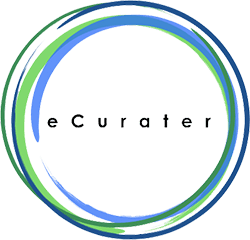
A 65-year-old male, diagnosed case of CA-PFS (locally advanced disease) treated with CTRT in 2018, was disease free for 1year, developed cough and pain over the chest wall. Whole body fluoro-deoxy glucose positron emission computer tomography (WB FDG PET CT) was performed which was suggestive of B/L lung nodules and small lesion in the left kidney. Biopsy from the lung and the renal mass was suggestive of metastatic squamous cell carcinoma. Immuno histochemistry was done and tumour cells showed to be diffusely and strongly positive for CK5/6 and negative for PAX8 and CK20. GATA3 was predominantly negative with focal weak positivity in some cells (Figure 1) suggestive of head and neck primary. The patient received 6 cycles of 1st line palliative chemotherapy paclitaxel 175mg/m2 and carboplatin AUC 5 X 6 cycles 3 weekly regimens. Post 6 cycles WB FDG PET CT was suggestive of progressive disease. The patient further received 3 cycles of immunotherapy Nivolumab 480 mg 4 weekly regimens. The response assessment WB FDG PET CT was suggestive of progressive disease; the size of the lesion of the left upper pole kidney increased from 2.9×3.2×5.1cm standard value uptake (SUV) of 9.0 to 4.7×6.4×5.8cm (SUV 11.4) along with the involvement of left renal hilum and para-aortic nodes (Figure 2). The patient developed pain in the left loin and was having restriction of movement. Hence was planned for palliative radiotherapy. The patient received palliative SBRT 25 Gray (Gy) /5 fractions to the left kidney mass in the upper pole, left para aortic mass on Elekta versa HD machine, treatment was planned on Monaco treatment planning system (Figure 3). To reduce the motion errors, active breath control (ABC) technique was used. The patient was assessed for acute toxicity, was followed up 15 days, 1 month after completion radiotherapy. The patient was symptom-free at the end of one month follow-up. The patient was continued on Nivolumab. The patients WB FDG PET CT were done for response assessment after 3months of completion of radiotherapy. The lung nodules were still present with stable disease, but the left renal mass had completely resolved completely (SUV- 2.2) (Figure 4).
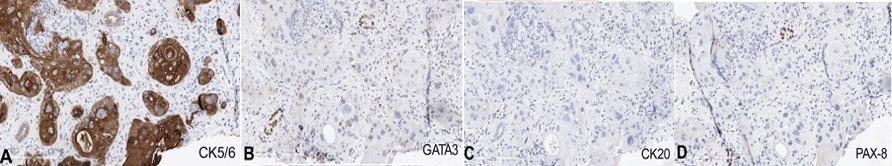
Figure1: Immunohistochemistry CK5/6, GATA3, CK 20 and PAX 8.
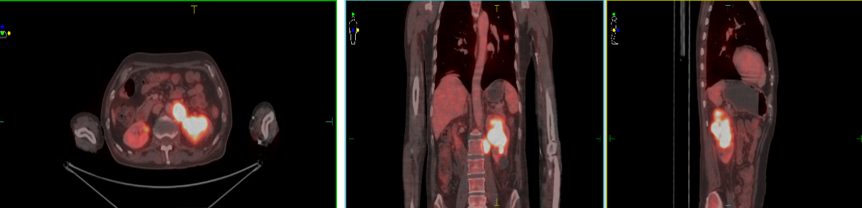
Figure 2: WB FDG PET CT showing increased uptake left kidney.
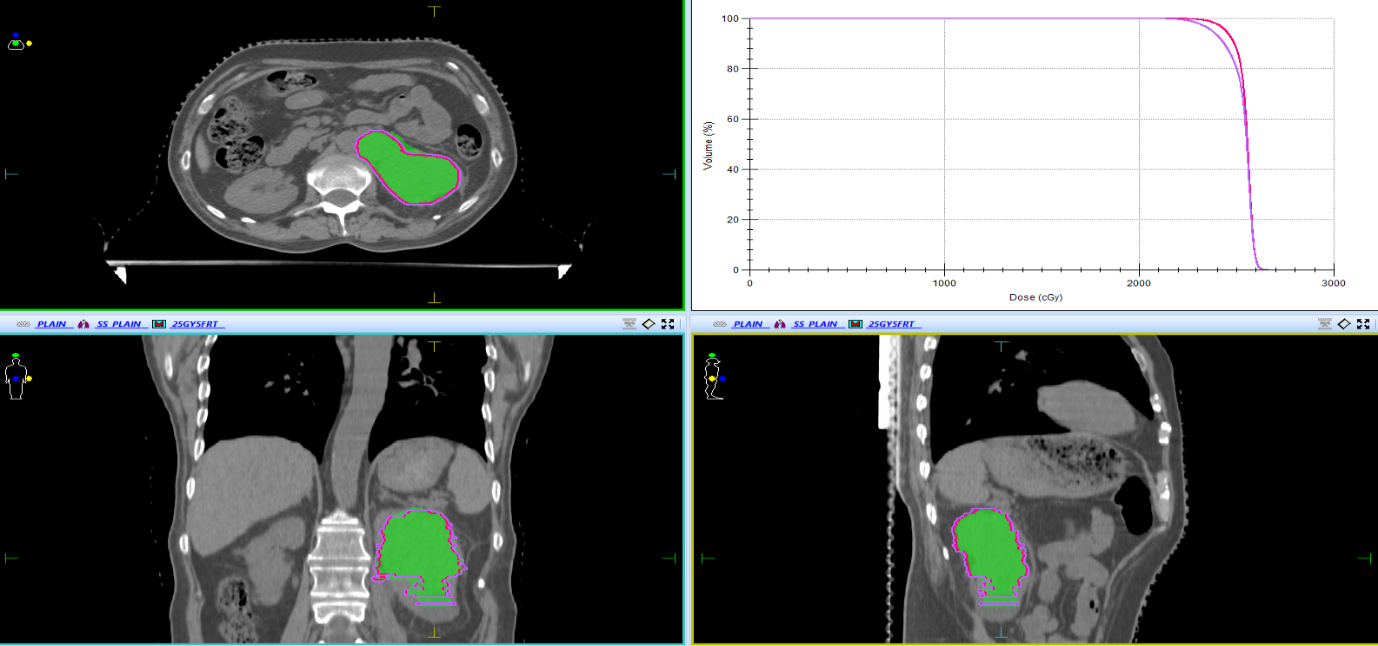
Figure 3: Treatment plan showing 100% dose delivered to Planning target volume (PTV). The isodose lines shown are dose delivered to Gross tumour volume (GTV) and Planning target volume (PTV) receiving 100% dose.
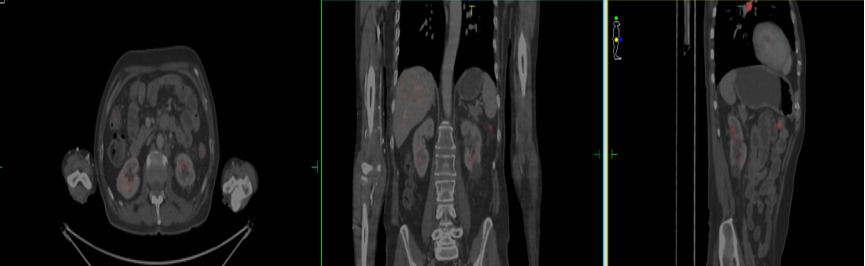
Figure 4: WB FDG PET CT shows near complete radiological resolution of the Left renal mass (SUV 2.2).
Discussion
Head and neck cancers are the most common cancers in males in India. The incidence of distant metastasis in head and neck cancers is about 15-25% as per the literature available [2]. The incidence of metastasis is in the following order: lungs being the most common primary site of metastasis, followed by liver, bones, adrenal and kidney. The renal metastases do not present with any clinical symptoms. According to literature, renal metastatic tumours are mainly located in the cortical zone close to the glomerular vascular plexus and seldom spread to urothelial tissue, so that the incidence of microscopic haematuria is 12% ~ 31% [3].
Retrospective studies done on renal metastasis from different primaries have shown that 6% of the primary is due to head and neck malignancies; the most common primary being Lung accounting for about 80%. In this series, over 50% of the patients were asymptomatic at presentation and 30% had flank pain. 77.5% had solitary involvement of the kidney. 32% of the patients underwent nephrectomy of the patients underwent nephrectomy. The median survival was about 14 months. There was no survival benefit in patients undergoing surgery. 8 out of nine patients with head and neck malignancies underwent surgery [4]. In our case, the patient had undergone CTRT, following which the patient developed lung metastasis. The patient received palliative chemotherapy, progressed with a small lesion in the left kidney, was started on immunotherapy Nivolumab, the
lesion in the lung and kidney progressed (Figure 2). The patient had pain in the left flank. The biopsy was done and IHC was suggestive of metastatic squamous cell carcinoma from the pyriform fossa.The patient was not willing for nephrectomy. Hence, the patient was planned for palliative SBRT. In stage IV and oligo-metastatic disease, SBRT is being frequently used in the recent past. This is generally preferred due to relatively low toxicity rates and higher local control in selected groups of patients. This has not only improved the local disease free progression, also has improved overall survival [5-12].
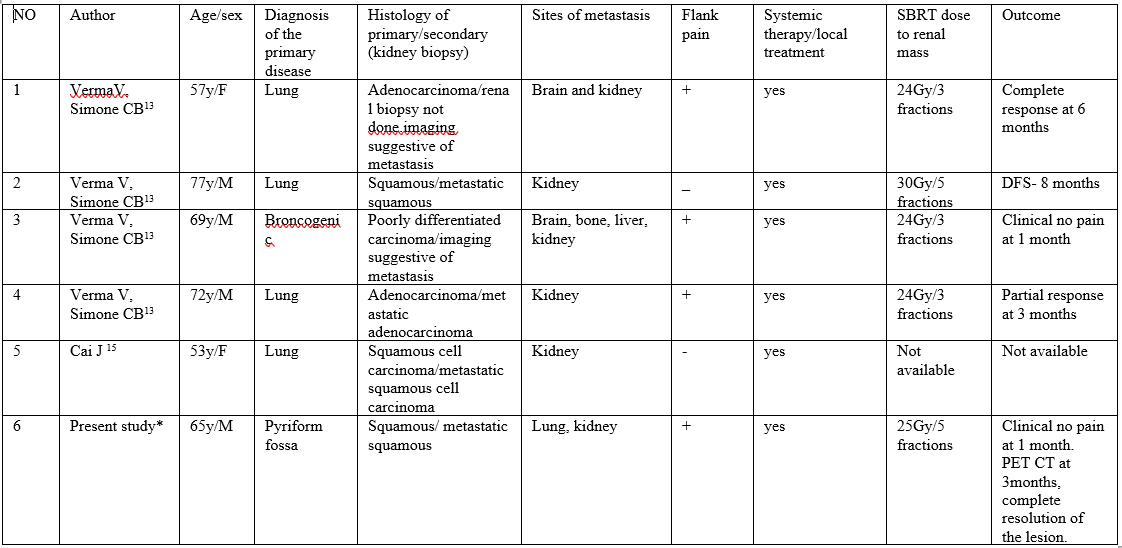
There is no enough data to suggest if SBRT is an effective form of treatment in patient with renal metastasis from other primaries. Case series published by Verma V and Simone CB, is the only data available for SBRT for renal metastasis from lung primary [13] (Table 1).
Table 1: Renal Metastasis treated with Stereotactic body radiotherapy (SBRT).
Hypo-fractionated palliative radiotherapy is practiced especially by using two-dimensional (2DRT) and three-dimensional radiotherapy (3DCRT) in low resource settings. This is associated with significant toxicity to surrounding structures like the small bowel, liver, and pancreas which gets irradiated when treatment is being delivered. Clinically, the patient develops significant nausea, vomiting and loose motion. With the advent of better and highly conformal radiation techniques, it is possible to deliver high ablative doses of radiation in single or multiple fractions to tumours with minimal doses to the surrounding normal structures. This significantly reduces acute toxicities during the course of treatment as well as reduces significant long term morbidities. This provides the best palliation and also the treatment is completed in a short period of time. The usual SBRT dose used for renal metastasis is 25Gy in three to five fractions. In our case, the patient received palliative SBRT 25Gy in 5 fractions to the left renal mass along with the renal hilum and para-aortic mass (Figure 3).
One of the other challenges faced during delivery of such high doses of radiation is the margin of error is very minimal and tumour miss can result in devastating results with significant toxicity to the surrounding structures. Organ motion is due to respiratory movements of the diaphragm. The kidney is fixed to the retroperitoneal fascia and the gerota’s fascia. The motion of the kidneys during free breathing is about <10mm in the anteroposterior and lateral directions with free breathing [14,15]. To address this issue, ABC technique was used wherein the patient is asked to hold the breath in deep inspiration for a fixed time of 10-15 seconds and treatment is delivered only during this phase and the process is repeated every after every 1-2 minutes of rest.
This has to be accounted for during planning to prevent geographic misses. The gross tumour volume (GTV) was contoured and a planning target volume (PTV) of an additional 2 mm was given. The 100% iso-dose to GTV volume was achieved as in Figure 2. The patient was treated with 25Gy/5 fractions.The patient did not have any toxicity during the course of the treatment. At 15 days and one month of follow-up the patient was stable; there was no pain. The patient was not on any analgesics for pain control. Three months following completion of treatment, the patient had complete resolution of the left renal mass (Figure 4).
Conclusion
Renal metastasis from head and neck malignancies is very rare. Therefore, as there is no added survival benefit with nephrectomy and in patients not willing for surgery, SBRT can be considered as a non-invasive option for palliative treatment. SBRT to kidney is well tolerated without any significant morbid side effects.
References
- Ferlay J, Soerjomataram I, Ervik M, Forman D, Bray Fet al. (2012) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136:E359-386.
- Ferlito A, Shaha AR, Silver CE, Rinaldo A, Mondin V (2001) Incidence and sites of distant metastases from head and neck cancer. ORL J Otorhinolaryngol Relat Spec 63:202-207.
- Bailey JE, Roubidoux MA, Dunnick NR (1998) Secondary renal neoplasms. Abdom Imaging 23:266-274.
- Zhou C, Urbauer DL, Fellman BM, Tamboli P, Zhang M, et al. (2016) Metastases to the kidney: a comprehensive analysis of 151 patients. BJU Int 117:775-782.
- Bedard G, McDonald R, Poon I, Erler D, SolimanH, et al. (2016) Stereotactic body radiation therapy for non-spine bone metastases–a review of the literature. Ann Palliat Med 5:58-66.
- Knisely J, Sahgal A, Lo S, Ma L, Chang E (2016) Stereotactic radiosurgery/ stereotactic body radiation therapy-reflection on the last decade’s achievements and future directions. Ann Palliat Med 5:139-144.
- Jones JA, Simone CB 2nd (2014) Palliative radiotherapy for advanced malignancies in a changing oncologic landscape: guiding principles and practice implementation. Ann Palliat Med 3:192-202.
- Siva S, MacManus M, Ball D (2010) Stereotactic radiotherapy for pulmonary oligometastases: a systematic review. J Thorac Oncol 5:1091-1099.
- Baumann BC, Nagda SN, Kolker JD, Levin WP, Weber KL, et al. (2016) Efficacy and safety of stereotactic body radiation therapy for the treatment of pulmonary metastases from sarcoma: A potential alternative to resection. J Surg Oncol 114:65-69.
- Patel AN, Simone CB 2nd, Jabbour SK (2016) Risk factors and management of oligometastatic non-small cell lung cancer. Ther Adv Respir Dis 10:338-348.
- Iyengar P, Kavanagh BD, Wardak Z (2014) Phase II trial of stereotactic body radiation therapy combined with erlotinib for patients with limited but progressive metastatic non-small-cell lung cancer. J Clin Oncol 32:3824-3830.
- Gomez DR, Blumenschein GR Jr, Lee JJ (2016) Local consolidative therapy versus maintenance therapy or observation for patients with oligometastatic non-smallcell lung cancer without progression after first-line systemic therapy: a multicentre, randomised, controlled, phase 2 study. Lancet Oncol 17:1672-1682.
- Vivek V, Charles B. Simone I (2017) Stereotactic body radiation therapy for metastases to the kidney in patients with non-small cell lung cancer: a new treatment paradigm for durable palliation. Ann Palliat Med 6:96-103.
- Pham D, Kron T, Foroudi F (2014) A review of kidney motion under free, deep and forced-shallow breathing conditions: implications for stereotactic ablative body radiotherapy treatment. Technol Cancer Res Treat 13:315-323.
- Cai J, Liang G, Cai Z (2013) Isolated renal metastasis from squamous cell lung cancer. Multidiscip Respir Med 8:2.
*Corresponding author: Murali Paramanandhan, Department of Radiation Oncology, Fortis Hospital, Bannerghatta Road, Bangalore.
Citation: Murali Paramanandhan (2022) Renal Metastasis in Carcinoma Pyriform Fossa treated with SBRT: A Case Report and a Brief Review.Arch Cancer Res Med 2: 002
Received: May 20, 2022; Accepted: June 19, 2022; Published: June 29, 2022
Copyright: © 2022 Murali Paramanandhan. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits un-restricted use, distribution, and reproduction in any medium, provided the original author and source are credited.