The Cardiac Surgeon’s Magic Weapon Once Again Comes Handy
- Article
- Article Info
- Author Info
Introduction
The occurrence of a primary cardiac malignancy is quite infrequent as per the available literature. The diagnosis is usually incidental and the treatment strategy is multidisciplinary. An unusual case of such a malignancy and management with a rare surgery is reported here.
Case Report
A 52-year-old female was admitted in our department with the complaints of class II dyspnoea on exertion. She had a previous history of cerebrovascular accident 3 months back. A computed Tomography (CT) of the brain revealed a Sub-acute non-haemorrhagic infarct of the Right Middle cerebral artery territory. Auscultation revealed a mid-diastolic murmur and a tumor plop in the mitral area. The roentgenogram and cardiogram was normal. She was investigated further with an echocardiogram which showed a large mobile mass of 7 x 8 cm in the left atrium (LA) causing left ventricular inflow obstruction during diastole [Figure 1A]. The CT chest supported the same findings. A plan for surgical removal of the mass was made. After midline sternotomy and cardiopulmonary bypass (CPB) the heart was arrested with cold blood cardioplegia.
The left atrium was opened through the interatrial groove. The mass was gelatinous with multiple fronds on its edges and posterosuperiorly occupying the orifice of the left pulmonary veins [Figure 2A].
Major part of the mass was excised and the mass was debulked. Inspite of extensive resection the mass still had its attachment on the posterior wall of LA and the left pulmonary veins. We were in a situation to decide between complete excision of the mass along with the posterior wall of LA, but removing the mass from the pulmonary vein orifice was a difficult task as the major part of pulmonary vein has to be removed and will leave the pulmonary veins to be deficient to the LA. Now this situation can be correlated to the ancient war situation in one of the great Indian epic “Mahabharata” where a weapon was used which doesn’t have any antidote and was considered as the last resort in any terminal situation. The weapon was named as “Brahmastra” which means a weapon created by God “Brahma”. Likewise, a magical weapon for a cardiac surgeon is nothing but the pericardium which comes as his last resort in any difficult situations. We made a crucial and prompt decision of using the pericardium for reconstructing the posterior wall of LA and the pulmonary venous orifices after resecting the mass along with the LA wall. The autologous pericardium was harvested and treated with 0.6% gluteraldehyde. This was trimmed in such a way to create a new posterior wall of LA and as well as accommodate the orifices of the left pulmonary veins. The mass was excised along with the posterior wall of LA and the left pulmonary veins. The treated pericardium was sutured with the native left atrium and the pulmonary veins using a 4-0 polypropylene suture and the LA was closed after ensuring the mitral valve competency [Figure 2B]. We were able to manage the procedure without any deep hypothermia or circulatory arrest. After weaning from Cardiopulmonary bypass and chest closure the patient was shifted to the Intensive postoperative care unit with inotropic supports. The mass was sent for histopathological investigation [Figure 1B].
The postoperative course was stormy. The patient was on prolonged ventilatory support for retained secretions and underwent a percutaneous tracheostomy for the same. The tracheostomy was weaned off on the 3rd week and the patient was shifted to the ward after stabilizing the hemodynamics. The post-operative echocardiogram showed normal sized LA chamber with normal functioning mitral valve. The patient was discharged with stable vitals and good general condition. The 3 months follow up scans were normal with the patient attaining better convalescence.
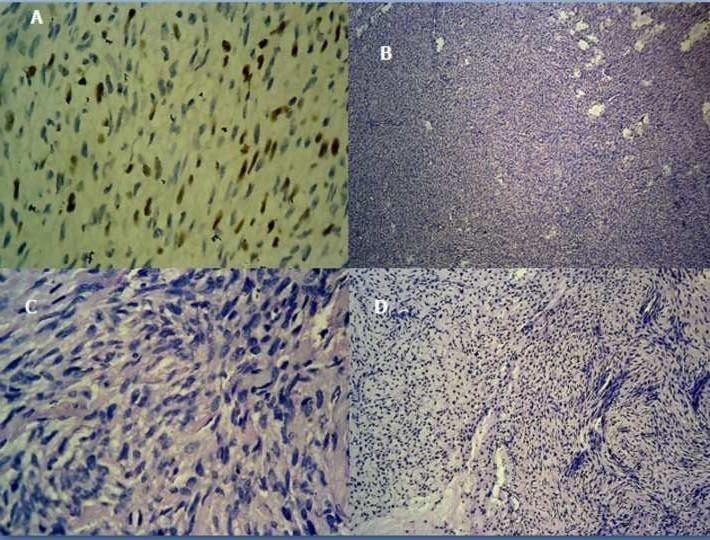
The histopathology of the mass revealed a low grade fibromyxoid sarcoma with desmin and smooth muscle actin positivity [Figure 3]. The margins of the pulmonary veins were negative for tumor cells. The patient and the attenders deferred any further oncological workup.
Figure 1: 1A- Echocardiogram showing a large mobile mass in the left atrium. 1B- Excised gelatinous mass with multiple fronds on its surface.

Figure 2: 2A- Illustrative diagram of the mass occupying the oricifes of the left pulmonary veins.
2B-Operative technique-The mass was removed along with the orifices of the left pulmonary veins and the trimmed treated pericardium is used to reconstruct the LA
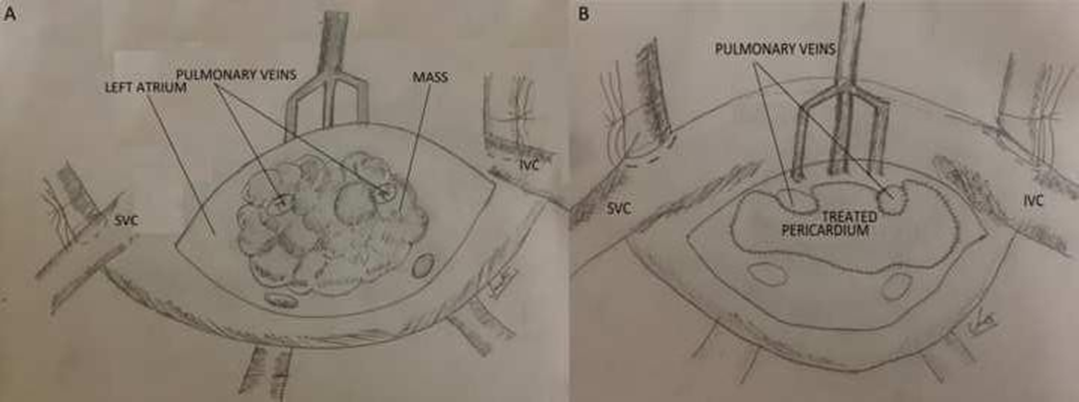
Figure 3: Histopathology showing a low-grade myxofibrosarcoma with Desmin, Smooth muscle actin and Ki 67 positivity.
Comment
Malignant masses of the cardiac chambers are extremely rare with a reported incidence of 0.001-0.03
% and are diagnosed when the tumor has already embolised or is metastasized to distant sites [1]. The common presentation is dyspnoea mimicking that of a valvular lesion or an obstructive cardiac lesion. Mostly the patients are asymptomatic and are diagnosed during routine health checkups or during an echocardiogram while evaluating for other diseases. The mass has the tendency to embolise to the brain as in this case or to other vital organs. The prognosis is poor when the mass has already been metastasized or embolised. Prompt diagnosis and early intervention once diagnosed can prevent the patient from morbid systemic side effects. The treatment of choice in large masses is surgical excision of the mass but not all tumors are amenable to complete resection owing to their extensive cardiac chamber invasion [2]. As reported by Shapira et al an extensive resection was carried out in this case as well but an autotransplantation was best avoided with our surgical expertise by the pericardial reconstruction of the LA in vivo [3,4]. Preoperative chemotherapy as described by Putnam and colleagues was not an option in our case as the mass has already embolised once which mandated an early surgical intervention [5]. Since we have achieved a complete (R0) resection and the margins of the pulmonary veins and the LA were negative for tumor cells on histopathology, we did not proceed with a postoperative chemotherapy.
Grandmougin et al and Coelho et al reported cardiac transplantation as a treatment option for major cardiac masses which was the last resort in our case [6].
Conclusion
Malignant Cardiac neoplasms can present with obstructive symptoms or even be asymptomatic and left undiagnosed. Once diagnosed they are either in the advanced stage or spread to other vital organs. When left untreated the prognosis is usually poor leading to embolisation symptoms and even death. The treatment of large masses includes radical excision and sometimes heart transplantation when there is extensive cardiac chamber invasion. Early diagnosis and intervention is the key to better survival.
Reference
- Mazuecos, JMJ, Manso F, Cubero JS, Ramos JT, Dominguez O, et al. (2003) Es util el transplante cardíaco como tratamiento del sarcoma cardiaco primario?. Revi Esp Cardiol. 56: 408– 411.
- Blackmon SH, Patel A, Reardon MJ (2008) Management of primary cardiac sarcomas. Expert Rev Cardiovasc Ther 6:1217-1222.
- Conklin LD, Reardon MJ (2002) Autotransplantation of the heart for primary cardiac malignancy: development and surgical technique. Tex Heart Inst J 29:105-8.
- Oz M. Shapira, Amit Korach, Uzi Izhar, Tomer Koler et al. (2013) Radical multidisciplinary approach to primary cardiac sarcomas. Eur J Cardiothorac Surg. 44: 330-336.
- Joe B Putnam, Jr, Michael S Sweeney, Rolando Colon, Louis A. Lama et al. (1991) Primary Cardiac Sarcomas.Ann Thorac Surg 51: 906-910.
- Pedro NP, Coelho, Nuno GMA, Banazol, Rui JM. Soares,José IG et al. (2010) Long-Term Survival With Heart Transplantation for Fibrosarcoma of the Heart. Ann thorac surg 90: 635- 636.
*Corresponding author: Dr. Sanath Kumar, MD, Meenakshi Mission Hospital and Research Centre Madurai, India. E-mail: kumarsanath@yahoo.com
Citation: Dr Sanath Kumar (2023) The Cardiac Surgeon’s Magic Weapon Once Again Comes Handy. Int J Card Carth Sur 2: 01.
Received: Nov 28, 2023; Accepted: Dec 08, 2023, Published: Dec 12 2023
Copyright: © 2023 Dr. Sanath Kumar. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits un-restricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sanath Kumar1*, Raghuram Arani 2, Kumar Subbaiyan3*, Prashant Kothari 4
Meenakshi Mission Hospital and Research Centre Madurai, India.