TWIDDLE`S SYNDROME: A RARE COMPLICATION OF PACEMAKER THERAPY: INITIAL ASSESSMENT WITH EVIDENCE BASED STUDY
- Article
- Article Info
- Author Info
Introduction
Twiddler`s syndrome is a rare but hazardous complication of cardiac pacemaker treatment.
Initially described by Bayliss et al.in 1968, Pacemaker twiddler`s syndrome (PTS) often occurs when a patient unintentionally or deliberately manipulates the pacemaker device, often leads to device displacement or pacemaker leads dislodgment which can result in device failure [1].
Globally PTS is considered a rare condition. It accounts for a small percentage of pacemaker-related complications. Most data come from individual case reports or smaller studies. Incidence of PTS to be between 0.1% and 1% of all pacemaker patients [2]. However, with the rising number of pacemaker and implantable cardioverter defibrillators (ICD) implantations worldwide, the potential risk of PTS has become more relevant.
European countries with advanced healthcare systems, such as the United Kingdom (UK), Germany and France, also report low incidence of PTS, but this may be underestimated due to lack of systematic screening [2]. Pacemaker use is increasing due to aging populations and improved access to cardiac care in Asia, and the rising number of pacemaker implantations suggests that PTS could become a more recognizable complication in the region [3].
In African continent low- and middle-income countries where access to advanced cardiac devices is growing, PTS may be under reported due to limited healthcare resources, lack of patient education, and inconsistent follow-up care. Pacemaker implantations are generally less frequent in these regions, but growing access to cardiac devices will likely increase PTS diagnosis in the future [4].In Kenya, PTS is rare, complication that occur in patents with pacemakers or implantable cardiac defibrillators (ICDs).
Symptoms of PTS are subtle; resembling other cardiac issues making it difficult to identify early [5] Research is needed to improve diagnostic protocols, emphasizing early recognition of tell-tale signs and symptoms.
Most of devices are easily manipulable by near normal activities as the modern pace makers are lighter and smaller aiding in dislodgement on manipulation within the pocket created during surgery [6].
The elderly are vulnerable to PTS due to increased subcutaneous tissue laxity and cognitive decline older patients also suffer dementia which impairs self-care post-surgery [7]. The aging process often makes the device more prone to movement within its surgical pocket and tacking to the wall with non-absorbable sutures and counseling is essential.
Materials & Methods
A 59-year-old female, re-admitted 8 months after pacemaker therapy, secondary to third degree heart block, the initial Pace maker therapy being in 2023. She reported of syncope episodes on and off and dizziness, generalized headache for one month. She was treated and discharged on medication as an outpatient without resolution. She also reports twitching of her right pectoral muscle for a day with no history of loss of consciousness and trauma.
Past medical history: No childhood-related cardiovascular illness, rheumatic fever, stroke or intermittent claudication.
Past surgical history-pacemaker insertion 2023
Drug history: She had a history of oral contraceptive use with no history of using recreational drugs and no reported drug allergies.no known food or drug allergies
Family history: No history of any related heart disease, hypertension or any other heritable cardiovascular risk factors.
General Examination
Patient was sick looking, Afebrile, no pallor, no jaundice, no lymphadenopathy, nor dehydrated or cyanosed.
Blood Pressure of 123/67mm/Hg, Pulse rate:-35B/m She had no lower limb Oedema.
Cardiovascular system: – S1 and S2 heart sounds were heard normal, no murmurs
Respiratory system: – Normal vesicular break sounds heard.
Gastro Intestinal system: -Soft, no tenderness or Organomegaly.
Genito- Urinary Tract:-Normal bowel movements, Central
Nervous System:- GCS 14/15, Not well oriented to time place and person
Vitals signs: Date Vitals Reference Range 14Th February 2023 BP 103/52mmHg Pulse 29b/min SPO2 89%.
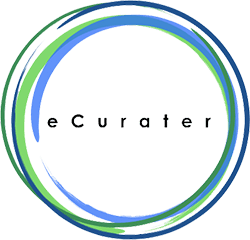
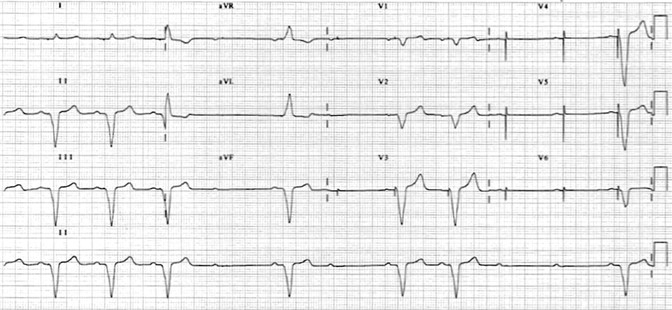
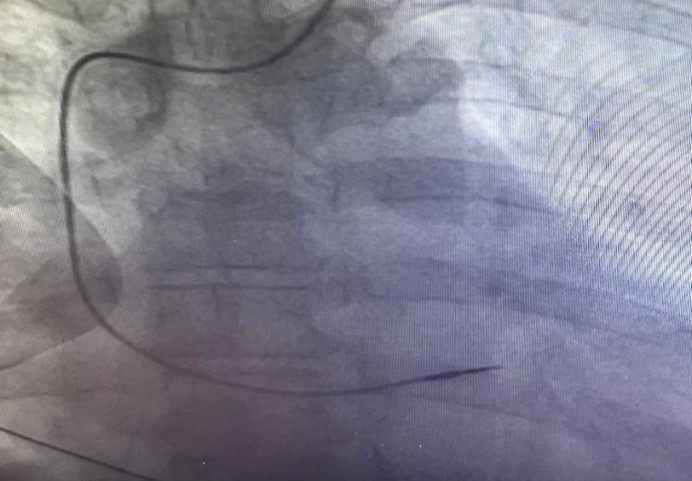
ECG at emergency department revealed loss of capture of pacemaker spikes [Figure 1]. Pacemaker interrogation showed complete loss of pacing and sensing of the ventricular lead. The patient admitted to any manipulation of the pace maker. Fluoroscopy revealed coiling of the pacing lead around the pulse generator [Figure 2]. The pacemaker pocket was reopened. Fortunately, both the insulation and the conductor of the lead were intact. The same lead was repositioned and proved to be functional with good pacing and sensing parameters [Figure 3]. The pulse generator was fixed on the pectoral muscle with non-absorbable sutures. No further complications were detected in one year follow-up.
Figure 1:
The ECG done on 14th February 2023, revealed loss of capture of pacemaker spikes (before or after).
Figure 2:
| Date | Vitals | Reference range |
| 14th February 2023 | BP 103/52 mmHg
Pulse 79b/min SPO2 89% |
<120/80
60-100 90-95% |
Laboratory investigations
14-02-2023
| UECs | Results | Reference range |
| Sodium | 133mmol | 145-150mmol |
| Potassium | 4.59mmol | 3.3-5.3mmol |
| Chloride | 104mmol | 99-110mmol |
| Urea | 8.9mmol | 2.6-7.0mmol |
| Creatinine | 136.66mmol | 50-120mmol |
| Liver functioning tests | Results | Reference range |
| Alkaline phosphatase | 119 UL | 35.360UL |
| Aspartate aminotransferase | 104 UL | 0.0-50UL |
| Gamma glutamyl transferase | 256 UL | 5-40UL |
| SGPT – Direct bilirubin | 81 | 11-50 |
| Prothrombin lime | 68.5 | 11-13.5 |
14-02-2023
| Diagnosis | Results | Reference image |
| CRP | 211.54 mg dl | 0.3-1.0mg dl |
| Uric acid | 456.34mmol | 149-339mmol |
| Random blood sugar | 7.7mmol | 3.3.7.8mmol |
| Cardiac troponin | 204ugl | 0-0.4ugl |
Details from a fluoroscopy showing the coiling of the pacing lead around the pulse generator of a pacemaker.
2A&2B: Pacemaker Defender Where both insolation and of the lead were intact.
2C&2D: The same lead was repositioned and proved to be functional with good pacing and sensing .
Discussion
Pacemaker Twiddler`s Syndrome (PTS) is a rare phenomenon typically observed in patients who have undergone cardiac pacing. It is characterized by the presence of two distinct pacemaker systems—one being a physiological, intrinsic rhythm and the other an artificial pacing rhythm from a pacemaker. This syndrome can be challenging to diagnose, especially when it occurs late in the patient’s management [8].
Patients present with symptoms that a can be attributed to other cardiac issues, such as fatigue, palpitations, or syncope. The coexistence of both pacemaker activity and intrinsic rhythm can lead to an irregular heart rhythm, making symptoms more difficult to interpret. Late diagnosis often occurs when there is a lack of awareness about PTS among healthcare providers, particularly in patients with a complex medical history or multiple comorbidities. Diagnosis typically relies on careful analysis of an electrocardiogram (ECG) to distinguish between the two pacing sources [9].
Pacemaker devices are prone to manipulation through factors such as movement of the body causing PTS, careful matching the size of the device pocket to the implanted device is essential. It is considerable to consider device manipulation when there is PTS. Older patients may have age-related cardiac changes, such as fibrosis and decreased responsiveness of the heart, which can complicate the interaction between intrinsic rhythms and pacemaker activity. Cognitive decline, which may affect understanding of their condition, symptoms, and the importance of adherence to follow-up care [9].
Understanding the roles of age, mental health, and education level in the context of Pacemaker Twiddler`s Syndrome is crucial for optimizing patient care. Addressing these factors can enhance patient outcomes, promote timely diagnosis, and improve management strategies for PTS [10].
Conclusion
Understanding Pacemaker Twiddler`s Syndrome is vital for improving patient outcomes. Late diagnosis poses significant risks. Increased awareness, proper diagnostic protocols, and ongoing education will enhance management of this syndrome [9].
Advancements in technology and design must prioritize adaptability and responsiveness to reduce the risks associated with PTS.
Understanding the roles of age, mental health, and education level in the context of Pacemaker Twiddler`s Syndrome is crucial for optimal patient care. This can enhance patient outcomes, promote timely diagnosis, and improve management strategies for PTS. Tailored education and interdisciplinary support are essential in helping patients navigate their care effectively [11]. Emerging technologies in future, aim to create more intelligent pacing systems that better understand and adapt to individual patient rhythms, potentially reducing the risk of PTS.
There is need to explore the possibility of modifying pacemaker designs or lead placement to minimize the risk of twiddling There is limited literature specifically addressing PTS available now.
References
- DeMarco DC, Xuereb RG (2016) Twiddling’s of the pacemaker results in lead dislodgement. Malta Med J: 21: 38–41.
- Castilo R, Cavusoglu E (2017) Twiddler’s syndrome: an interesting cause of pacemaker failure. Cardiology 105:119–121.
- Gupta AK, Burgos Claudio MI, Hus N (2020) Unusual delayed complication of pacemaker leads. Cureus 12: e9479.
- Mandal M, Pande A, Kahali D (2019) A rare case of very early pacemaker twiddler’s syndrome. Heart Views 13:114–115.
- Khattak F, Khalid M, Gaddam S, Ramu V, Brahmbhatt V (2018) A rare case of complete fragmentation of pacemaker lead after a high-velocity theme park ride. Case Rep Cardiol: 419296.
- Tahirovic E, Haxhibeqiri-Karabdic I (2018) Twiddler’s Syndrome: Case report and literature review. Heart Views 19: 27–31.
- Salahuddin, Mohammad Cader, Fathima Aaysha (2016) The pacemaker twiddler’s syndrome: an infrequent cause of pacemaker failure. BMC Research Notes 9 (1).
- Mohsen Inbar, Shmuel, Neckels, Brenda Shook, Heather (2005) Twiddling to the extreme: development of twiddler syndrome in an implanted cardioverter-defibrillator. J Invasive Cardiol 17: 195–196.
- Bayliss CE, Beanlands DS, Baird RJ (1968) The pacemaker-twiddlers syndrome: a new compilation of implantable transvenous pace makers. Can Med Asscoc J 99: 371-373.
- Nicholson WJ, Tuohy KA,Tilkemeier P (2003) Twiddlers syndrome. N Engl J Med 348: 1726-1727.
- Gupta R, Lin E (2004) Twiddler syndrome. J Emerg Med 26:119-120.
1Head of Dept. of clinical medicine and surgery, Karen Training college
2Clinical Cardiology student
3Chief Cardiothoracic & Vascular Surgeon
4Cardiology program coordinator and instructor
5Interventional Cardiologists
6Senior Cardiologist
7Clinical cardiology student.The Karen Hospital,Nairobi, Kenya
8Pediatric Cardiologist, Chairman of The Karen Hospital
Masese CO1,Gachoka J2, Ponoth P3,Timothy TM4,Gikonyo AK5,Gikonyo D6,Gatwiri W7, Gikonya BM8
*Corresponding author: Dr. Charles O.Masese, The Karen Hospital Medical Training College, Langata Road,Karen, Nairobi. Email Adress: Charlesmasese49@gmail.com
Citation: Dr Charles O.Masese (2025) Twiddle`S Syndrome: A Rare Complication of Pacemaker Therapy: Initial Assessment with Evidence Based Study. Int J Card Carth Sur 5: 01.
Received: Sep 05, 2025; Accepted: Sep 15, 2025, Published: Sep 22, 2025